
Ventricular rhythm arising more distally in the Purkinje plexus of the left ventricular myocardium displays the pattern of right bundle branch block, and those of right ventricular origin display the pattern of left bundle branch block. Rhythms arising in the anterior or posterior fascicle of the left bundle branch exhibit a pattern of incomplete right bundle branch block with left posterior fascicular block and left anterior fascicular block, respectively. An incomplete right bundle branch block is seen when the pacemaker is in the left bundle branch. The rhythm has variable associations relative to bundle branch blocks depending on the foci site.Īn incomplete left bundle branch block pattern presents if ventricular rhythm arises from the right bundle branch block. Isorhythmic dissociation, fusion or capture beats can occur when sinus and ectopic foci discharge at the same rate. The idioventricular rhythm becomes accelerated when the ectopic focus generates impulses above its intrinsic rate leading to a heart rate between 50 to 110 beats per minute. With the slowing of the intrinsic sinus rate and ventricular takeover, idioventricular rhythm is generated. Subsequently, the ventricle may assume the role of a dominant pacemaker. Sinoatrial node and the atrioventricular node may get suppressed with structural damage or functional dysfunction potentiated by enhanced vagal tone.

The trigger activity is the main arrhythmogenic mechanism involved in patients with digitalis toxicity. Idioventicular rhythm has two similar pathophysiologies described leading to ectopic focus in the ventricle to take the role of a dominant pacemaker.Įctopic automaticity generated by abnormal calcium-dependent automatism that affects the diastolic depolarization, i.e., phase 4 action potential, is the main electrophysiological mechanism affecting the AIVR. The mechanism involves a decrease in the sympathetic but an increase in vagal tone. Īccelerated Idioventricular rhythm is also be rarely seen in patients without any evidence of cardiac disease.
Idioventricular rhythm can also infrequently occur in infants with congenital heart diseases and cardiomyopathies such as hypertrophic cardiomyopathies and arrhythmogenic right ventricular dysplasia. Various medications such as digoxin at toxic levels, beta-adrenoreceptor agonists like isoprenaline, adrenaline, anesthetic agents including desflurane, halothane, and illicit drugs like cocaine have reported being etiological factors in patients with AIVR. Įlectrolyte abnormalities can increase the chances of idioventricular rhythm. Idioventricular rhythm can also be seen during the reperfusion phase of myocardial infarction, especially in patients receiving thrombolytic therapy. It commonly presents in atrioventricular (AV) dissociation due to an advanced or complete heart block or when the AV junction fails to produce 'escape' rhythm after a sinus arrest or sinoatrial nodal block.
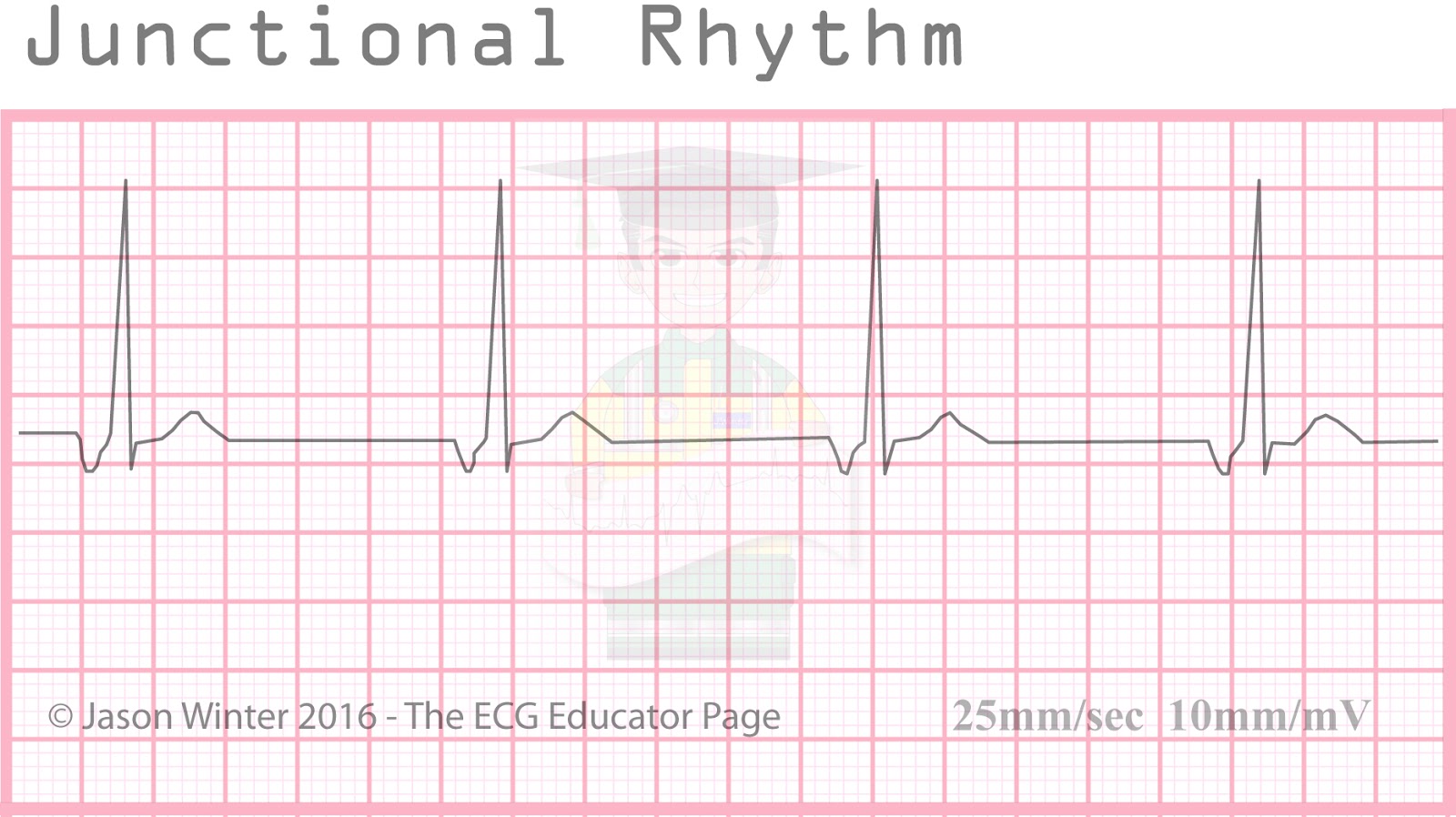
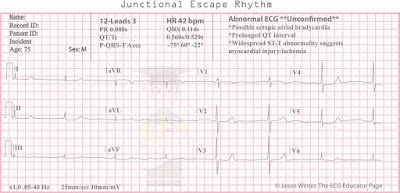
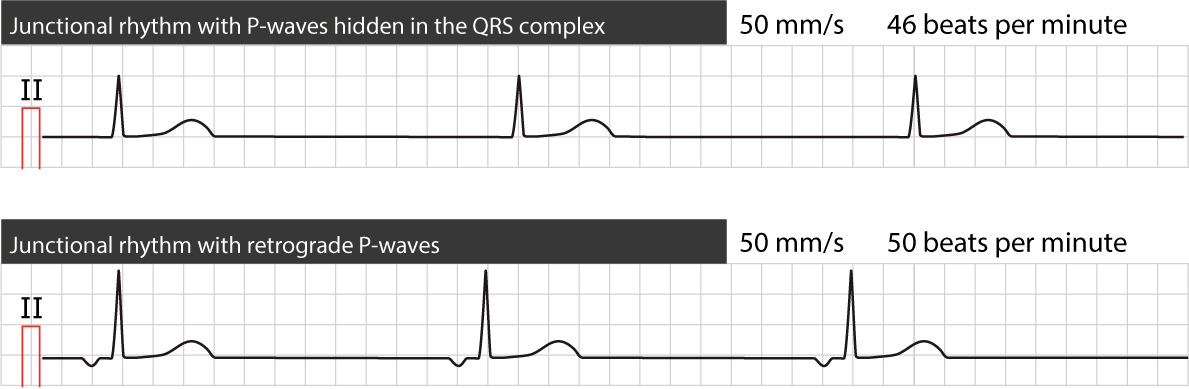
Idioventricular rhythm can be seen in and potentiated by various etiologies. It is a hemodynamically stable rhythm and can occur after a myocardial infarction during the reperfusion phase. Īccelerated idioventricular rhythm (AIVR) results when the rate of an ectopic ventricular pacemaker exceeds that of the sinus node with a rate of around 50 to 110 bpm and often associated with increased vagal tone and decreased sympathetic tone. Idioventricular rhythm is similar to ventricular tachycardia, except the rate is less than 60 bpm and is alternatively called a 'slow ventricular tachycardia.' When the rate is between 50 to 110 bpm, it is referred to as accelerated idioventricular rhythm. When ventricular rhythm takes over, it is essentially called Idioventricular rhythm. When the sinoatrial node is blocked or suppressed, latent pacemakers become active to conduct rhythm secondary to enhanced activity and generate escape beats that can be atrial itself, junctional or ventricular. Idioventricular rhythm is a slow regular ventricular rhythm, typically with a rate of less than 50, absence of P waves, and a prolonged QRS interval.


 0 kommentar(er)
0 kommentar(er)
